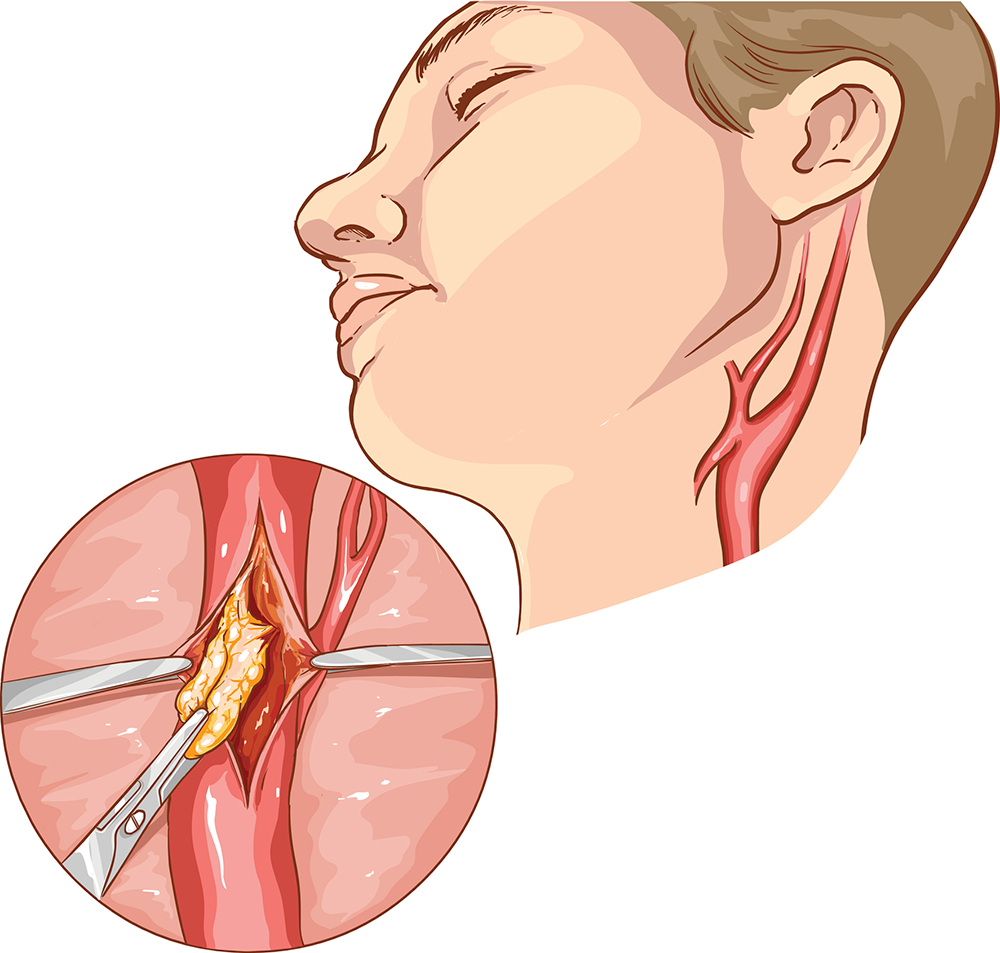
A carotid endarterectomy (CEA) is a surgical procedure to remove potentially dangerous plaque from within the carotid artery. It is a procedure performed by a board-certified vascular surgeon, like the ones we have at The Cardiovascular Care Group.
The plaque removal is primarily done to prevent a patient from having an initial or potentially fatal stroke, or to prevent those who may have recently had a stroke or Transient Ischemic Attacks (TIA) from having another, more devastating stroke.
Plaque is essentially the buildup of calcium deposits, also known as the hardening of the arteries (atherosclerosis). Plaque within the carotid artery can either narrow (stenosis) or completely block (occlude) the artery, or dislodge (embolize) and travel to the small arteries within the brain, thus causing a stroke.
How to Get Rid of Plaque
The first line of defense against this plaque buildup is preventive medicine. Patients are often placed on cholesterol-lowering medication (such as a statin) and aspirin to reduce the continued buildup. Patients are also encouraged to stop smoking immediately, as tobacco abuse has been shown to speed up the buildup of this plaque within the arteries.
The vast majority of patients with carotid plaque do not require an intervention. It is only when a patient exhibits symptoms such as a Transient Ischemic Attack (mini-stroke) or recovers from a recent stroke and is found to have a high grade stenosis (narrowing) in the carotid artery that feeds the side of the stroke, is a carotid endarterectomy recommended. This is an absolute indication for carotid endarterectomy.
CEA is also done as a preventive procedure in those patients who have a significant stenosis in their carotid arteries (greater than 70-80%), as the risk of stroke is higher in those patients than treating them with medicine alone. Your vascular surgeon will discuss the risk and benefits for carotid surgery if your carotid arteries are diseased.
Performing a CEA
Carotid endarterectomy is performed in a hospital setting and patients are usually admitted the day of surgery. The patients are taken to the operating room and may be put under general anesthesia for the operation. There are times when this procedure is done under local-regional anesthesia (twilight sleep). The type of anesthesia used depends on your surgeon’s preference, your medical history and the anesthesiologist’s comfort level with each. There is no difference in procedure outcomes and both types of anesthesia are acceptable and are well established in performing CEA.
Once anesthesia is given, a small skin incision is made overlying the carotid artery in the neck and the underlying muscle and vein are pushed to the side and the carotid artery is exposed. Vascular clamps are placed on the carotid artery to stop the flow of blood and the artery is opened. Depending on the type of anesthesia used and the technique used, a temporary “shunt” may or may not be necessary to get blood flow to the brain during the brief time that the carotid artery is clamped. The hardened plaque is then lifted and removed from the artery wall and the opening of the artery is closed with small sutures and a patch to reduce the chances of the narrowing reoccurring. The neck incision is then closed with absorbable sutures and a dressing placed.
What to Expect After a Carotid Endarterectomy (CEA)
Once awoken from the anesthesia, patients are observed overnight at the hospital. Most patients are subsequently discharged the morning after surgery. Some patients may require intravenous medicine to control their blood pressure during the early hours following surgery as the body “resets”. Patients may also have small drains left in overnight to help prevent blood from being trapped under the incision and this is usually removed prior to discharge.
Once discharged from the hospital, a patient may experience some mild neck stiffness and swelling. These are normal findings following a CEA. Some numbness overlying the side of the neck where the incision was made is not an uncommon finding and typically resolves over time. Patients are advised not to drive for 5-7 days after surgery or until they are comfortable turning their necks from side to side. A follow-up appointment with the surgeon is scheduled in 7-14 days post-operatively. Patients should call their doctor if they experience increasing swelling in the neck, prolonged headaches or neurologic symptoms. Although rare, these may be signs of a potentially dangerous situation.
At the first post-operative visit, the patient’s wound is checked and the neurologic status is evaluated. They are then scheduled for a baseline carotid ultrasound to monitor the status of the carotid artery after carotid endarterectomy and this is repeated every 6 – 12 months. Patients typically resume their normal activity within 2 weeks of surgery. Continued lifestyle modifications, such as refraining from smoking, good blood pressure control, healthy eating and exercise all help in reducing the risk of recurrent stenosis of the carotid arteries.
If you would like to know if you are a candidate for CEA or want to better understand your levels of potential plaque, schedule an appointment with one of our vascular surgeons today.






.jpg?width=944&name=Castle-Connolly-Top-Doctors-Emblem-Large%20(4).jpg)