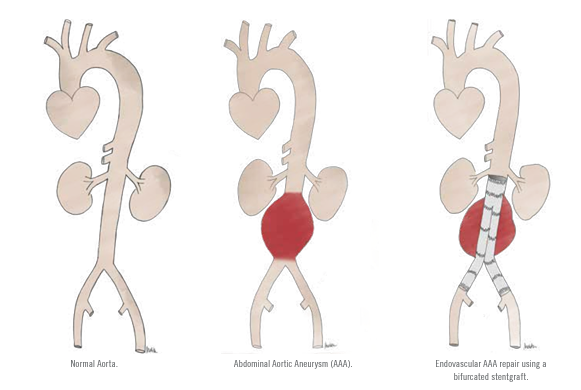
Endovascular abdominal aortic aneurysm repair (EVAR) is a minimally invasive alternative to conventional open surgical repair, and is generally indicated for abdominal aortic aneurysms (AAA) that reach 5 cm in maximum diameter.
In these procedures, access to the AAA is obtained via the femoral arteries at the
level of the groin crease. This can usually be accomplished by percutaneous means, although sometimes requires small incisions in the groin crease. Following femoral artery access, the vascular surgeon navigates wires and catheters within the blood vessels across the aneurysm using fluoroscopic (X-Ray) guidance.
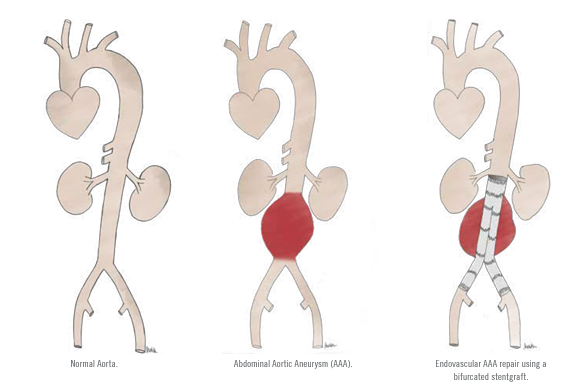
EVAR involves placement of an expandable stentgraft within and across the AAA and its primary purpose is to exclude the weakened wall of the AAA from systemic arterial pressure. The vast majority of currently available stentgrafts are composed of a synthetic fabric supported by a metal mesh framework that looks like a pair of pants with a waist and 2 legs. Stentgrafts are packaged within a delivery sheath that is used to navigate from the femoral arteries into and across the AAA. These appropriately sized devices are deployed and expanded within healthy native aorta above, and in the healthy iliac arteries below the AAA. Once fully deployed, the stentgraft diverts blood flow and takes the pressure off the aneurysm, thus reducing the risk of growth and rupture.
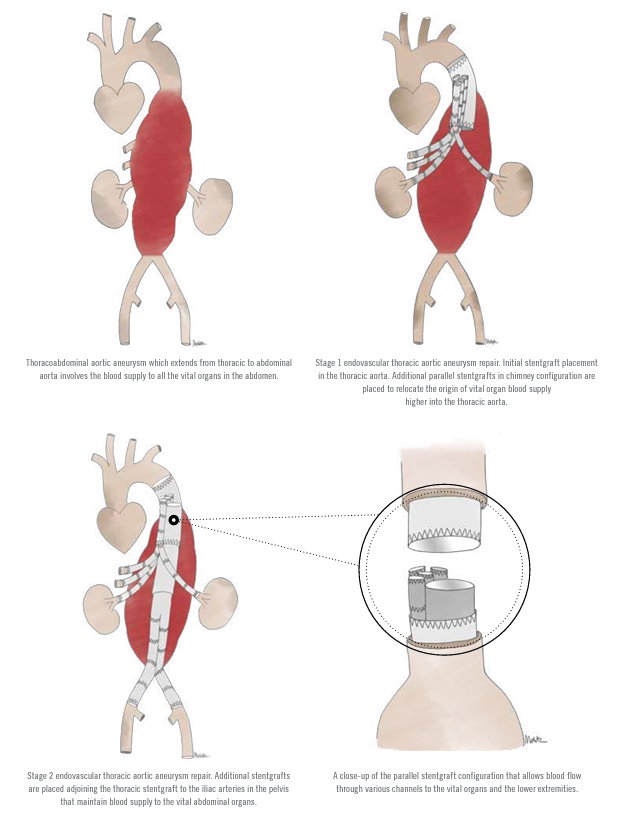
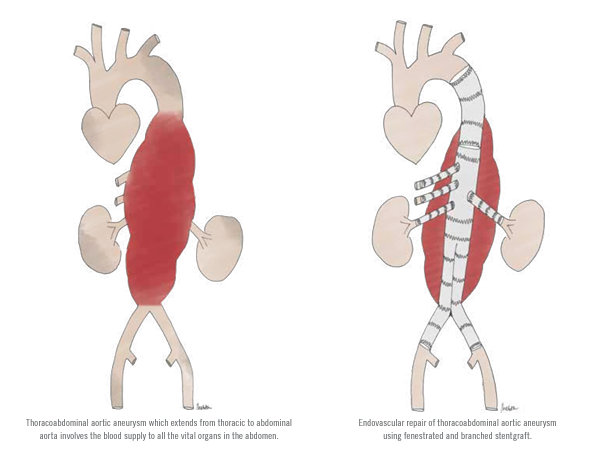
Patients with complex AAA that involve the origin of visceral arteries that supply vital abdominal organs including the liver, bowel, kidneys, etc., can also be successfully managed with EVAR. As the complexity of AAA increases, so does the makeup of the stentgrafts needed to treat them. Vascular surgeons often utilize devices with fenestrations, branches, and chimneys to accommodate and provide adequate blood flow to the visceral arteries while excluding the AAA. Such devices will allow surgeons to treat complex aneurysms that are extensive and involve blood flow to the liver, kidneys, and bowels.
The fenestrations, branches, or chimneys allow preservation of blood flow to the vital internal abdominal organs while diverting blood flow away from the aneurysms. During the endovascular procedures, the stentgraft fenestrations, branches, and/or chimneys are aligned precisely with the origins of the arteries that extend from the aorta to provide blood flow to vital organs in the abdomen. Special stents designed to keep these arteries open are then navigated through the stentgrafts and used to anchor the stentgraft fabric to the origins of these vital arteries. The sequence of these maneuvers requires precision within millimeters, and the surgeons navigate these devices with enhanced three-dimensional imaging in the operating room. In the not too distant future, further enhancements in imaging and robotics technology are sure to play a major role in improving these procedures even further.
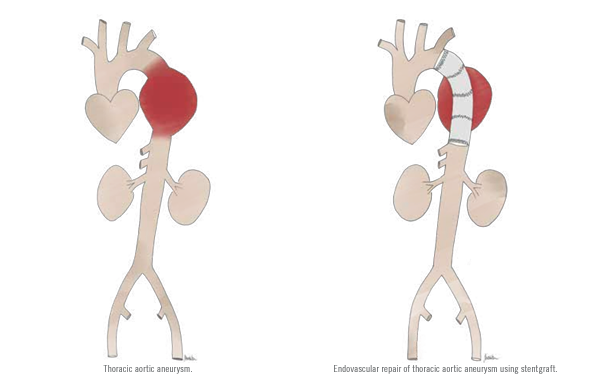
Similarly, when patients present with thoracic aortic aneurysms and dissections, endovascular repair requires the vascular surgeons to gain remote access to the aorta through femoral arteries in the groin. Under x-ray guidance,
the surgeon/operator navigates wires, catheters, and stentgrafts within the arteries and places the stentgraft strategically in healthy aorta above and below the dissections, thereby excluding blood flow within the torn false lumen. Depending on the extent of the aortic dissection, adjunctive endovascular and/or hybrid surgical procedures are sometimes required to maintain vital organ perfusion and thrombosis of the dissected aortic false lumen.
Choosing Treatment
Over the past 2 decades, endovascular technology has had a substantial impact on our ability to treat patients with aortic aneurysms and dissections. In the United States, approximately 250,000 patients each year are diagnosed with aortic aneurysms and dissections. Of these, nearly 1/3 will receive treatment, and the vast majority will undergo minimally invasive endovascular procedures. Pre-procedure planning is critical for technical success, and the vascular surgeon will routinely evaluate the patient presentation, aortic anatomy, and pre-existing medical conditions to determine whether they qualify for minimally invasive or open surgical repair. These procedures are generally performed under general anesthesia, spinal or epidural anesthesia, or even local anesthesia. In patients who are considered suitable candidates, endovascular aneurysm repair has a technical success rate of over 98%. Complications affecting the heart, lungs, kidneys, bowels, and other organs generally occur in fewer than 10% of patients, and the chance of death is approximately 1%. Most patients recover in the hospital for 1-2 days and return to their normal baseline activities in a few weeks. There are several possible complications of endovascular aneurysm repair that may require additional secondary intervention. Endoleaks are the presence of persistent blood flow in the aneurysm sac due to inadequate stentgraft seal or back-bleeding from small collateral blood vessels originating in the aortic aneurysm. Stentgraft migration can occur over time and may lead to endoleaks from stentgraft seal zones above and below the aneurysm. The development of other aortic and iliac aneurysms and failure of stentgraft integrity may also call for additional treatment in 15-20% of patients. It is for these reasons that following endovascular aneurysm repair, patients need to stay connected to their vascular surgeon in order to undergo routine follow-up and be treated appropriately for any issues that might arise. Minimally invasive endovascular treatment strategies for aortic dissections have transformed how we manage patients with complicated and uncomplicated aortic dissections, leading to significant reductions in patient morbidity and mortality. Prompt diagnosis and mobilization of appropriate surgical teams, however, remain critical for optimum patient outcomes.
Minimally invasive endovascular treatments have become mainstream for managing elective and emergent aortic aneurysms and dissections and have transformed how we manage patients with these complex aortic problems.
For more information and to schedule a consult, please contact us.
This article is a V-AWARE Property. Center for Vascular Awareness, Inc. (www.myvascularhealth.org)







.jpg?width=944&name=Castle-Connolly-Top-Doctors-Emblem-Large%20(4).jpg)